The sexual side effects of psychiatric medications are troubling enough that some patients consider treatment cessation. The authors review 5 strategies for managing sexual dysfunction.
It has been said that individuals avoid discussing religion, politics, and money. In this article, we will address another taboo topic: sexual dysfunction (SD), which occurs when an individual has difficulty with 1 or more components of the sexual response cycle, presenting as decreased libido, early or delayed ejaculation, orgasmic dysfunction, impaired genital sensation, erectile dysfunction, and/or insufficient lubrication in women.1
SD is relatively common. In the general adult population, the estimated prevalence of SD is 20% to 30% in men and 40% to 45% in women.1 Certain risk factors may increase the risk, including psychiatric disease. For example, based on International Classification of Diseases, Tenth Revision (ICD-10) definitions, 74% of men and 82% of women with schizophrenia, reported at least 1 sexual problem.2 However, psychiatric patients experiencing SD are often hesitant to disclose concerns to health care professionals.2,3
Medicinal treatment of psychiatric diseases is also a significant cause of SD. Antidepressants, antipsychotics, and benzodiazepines are 3 drug classes that are potent etiologies of SD (Table 1).4-10 According to a validated survey for assessing SD (SalSex), nearly half of patients treated for a psychotic disorder developed SD.3 Another study suggested that 25% to 80% of patients treated with antidepressants developed SD.11 This is a major concern, as some patients have shown poor tolerance to the sexual side effects of psychiatric medications and have considered treatment cessation as a result.3,12 Furthermore, emerging evidence suggests that the sexual side effects of psychiatric medications persist even after medication discontinuation, causing patients great distress.13

SD is a significant concern for patients on psychiatric medications. However, SD is often inadequately addressed.
Medication Classes and Sexual Dysfunction
SELECTIVE SEROTONIN REUPTAKE INHIBITORS. Selective serotonin reuptake inhibitors (SSRIs) are commonly utilized in the treatment of major depression, anxiety disorders, posttraumatic stress disorder, and obsessive-compulsive disorder, among others.13 The prevalence of sexual side effects is not well defined. One post-market study estimated SD prevalence in patients treated with SSRIs between 5% and 15%,4 while some studies reported up to 80% of patients experienced sexual side effects.5 Although some patients experiencing sexual side effects may see their symptoms resolve over the course of treatment, the vast majority will continue to experience side effects during SSRI treatment.13 Some patients may continue to suffer from persistent side effects despite the discontinuing medication, a condition known as post-SSRI sexual dysfunction (PSSD).13 Although there is limited clinical trial data, available studies found the highest incidence of sexual side effects in patients treated with paroxetine, followed by fluvoxamine, sertraline, and fluoxetine.6,7
A proposed mechanism for SSRI-induced SD lies within the interaction between serotonin and 5-hydroxytryptamine receptors (5HT1A).13 SSRIs are hypothesized to cause downregulation of 5HT1A due to the persistent stimulation by serotonin and resulting epigenetic changes that have implications for regulation of sexual motivation. It is likely that other 5HT receptor subtypes are similarly affected. The effect of elevated serotonin on levels of other hormones and neurotransmitters that play an important role in sexual function, such as testosterone and dopamine, may also account for some of SSRIs’ sexual side effects. These effects appear to be dose-dependent, with higher doses increasing one’s risk of SD.14,15 Thus, providers must weigh the potential benefits of increasing drug doses with increasing risk of adverse effects.15
ANTIPSYCHOTICS. SD is a common adverse effect (present in up to 48% to 75% of patients) of both oral and depotantipsychotic medications.8,16 Results of a recent meta-analysis described SD prevalence in those treated with oral antipsychotics to be between 16% to 60%.9,17 Treatment with quetiapine (16%), ziprasidone (18%), and aripiprazole (27%) were associated with the lowest rates of SD. Olanzapine (40%), risperidone (43%), haloperidol (45%), clozapine (52%), and thioridazine (60%) were associated with higher prevalence of SD. In long-acting depot antipsychotics, first- versus second-generation antipsychotics are more strongly associated with SD.18,19
Sexual side effects can likely be traced to the disruption of various neurogenic and hormonal factors impacted by the antipsychotics.9 Mechanisms vary based on action of specific medications. For instance, antidopaminergic medications likely impact the dopaminergic activity of the mesolimbic system, which is integral to sexual functioning. Atypical antipsychotics that target postsynaptic 5HT receptors can negatively affect arousal, orgasm, and ejaculation, as serotonin inhibits sexual desire. Medications that influence levels of luteinizing hormone, follicle-stimulating hormone, prolactin, testosterone, or other neuroendocrine changes can lead to imbalance of these factors necessary for optimal sexual functioning. This was illustrated in the meta-analysis described previously, which generally showed prolactin-raising antipsychotics (eg, haloperidol) caused greater SD compared with prolactin-sparing drugs (eg, ziprasidone).17 Also, as with SSRIs, antipsychotic-based SD appears to be dose-related.9,20 Thus, to assess a patient’s risk of SD, providers must consider both the dosage and mechanism of a particular antipsychotic.
BENZODIAZEPINES. Benzodiazepines have been reported to result in SD, but this effect is less evident and less reported than the classes of drugs previously discussed. The results of a multicenter double-blind randomized comparative study of patients treated with acute phase alprazolam for panic disorder found that the benzodiazepines did not cause SD.21 Other studies point to increased sexual arousal because of reduced anxiety in patients treated with benzodiazepines.22 Conversely, 2 studies have reported anorgasmia in 25% to 50% of patient samples treated with alprazolam.10 It is possible that benzodiazepines may reduce anxiety-related aspects of SD while causing anorgasmia and/or other negative impacts on sexual function.
Although there is limited evidence of the mechanism behind the SD caused by benzodiazepines, contributing factors could include effects on neurotransmitters and drug-drug interactions. Benzodiazepines are allosteric modulators of the gamma-amino butyric acid (GABA)-A receptor.10 GABA, a central nervous system neurotransmitter, has been associated with decreased sexual behavior. Increased GABA activity could account for decreased sexual function. Benzodiazepines may also contribute indirectly to SD through increased concentrations of concurrently taken medications because of interactions with the cytochrome P450 system.10
Dysfunction in the Clinic
Mental health care professionals should take the lead in discussing SD with patients. Patients are often unable or unwilling to initiate a dialogue about sexual concerns, and SD could go unnoticed. For example, 1 study showed that 63% of patients experiencing sexual side effects from treatment but did not spontaneously report the issue.3 Importantly, 1 of 3 of those patients felt their dysfunction was significantly impacting their quality of life. An additional study revealed that 50% of patients rarely if ever discussed their SD with providers, even if it had affected adherence to treatment.23
The sexual effects of psychiatric medications should be communicated at 3 distinct times: before, during, and after treatment. It is often difficult to discern retroactively if a patient’s SD is from their mental health condition or their psychiatric medications. Thus, establishing a baseline level of sexual function before treatment is extremely helpful. Then, throughout treatment, the clinician should continuously follow up with patients on their sexual function either verbally or through the usage of validated questionnaires.24
If a patient is experiencing treatment-related dysfunction, it is important to ask how distressed the patient is by their SD.25 Not all patients with treatment-induced SD are greatly concerned about it.3,23 It may also be helpful to directly ask patients if their SD has ever caused them to cease their medications.
Finally, if patients complete treatment, it is important to follow up and inquire if their SD has resolved, as some patients experience lingering SD after discontinuation of treatment.13 It is therefore important to detect this and help patients seek appropriate therapies to treat their SD.
Managing Dysfunction
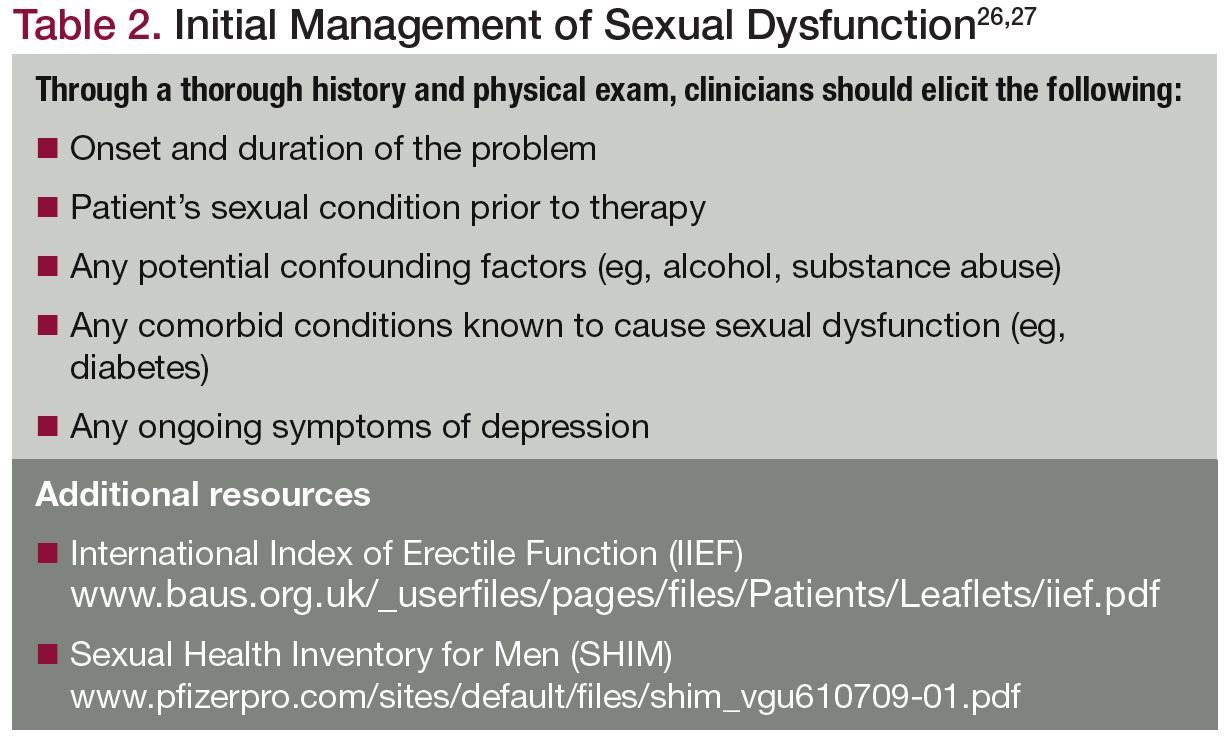
Irrespective of the presumed cause of SD, the initial management of patients presenting with SD symptoms must begin with a thorough history and physical exam to ensure that the SD is indeed a product of psychiatric medication use (Table 2).26,27 The clinician should also utilize validated psychometric questionnaires, such as the International Index of Erectile Function (IIEF) or its short version, the Sexual Health Inventory for Men (SHIM) (Table 2),at the initial and follow-up visits to assess the various sexual function domains (ie, erectile function, libido, orgasmic function, intercourse, overall satisfaction) at baseline and following initiation or modification of a specific treatment modality.27 Identifying reversible risk factors for SD, such as hypogonadism, hypertension, and obesity, and initiating appropriate treatment should be the clinician’s primary focus during the initial evaluation.27 It is only after addressing easily reversible risk factors for SD that a clinician should suspect psychotropic medications as the cause of SD, especially if the timing of SD remains unclear.
Given the lack of evidence-based treatments, management of patients with presumed psychotropic-induced SD proves to be more of an art rather than a science, and only 20% of prescribers discuss this topic with their patients.25 For the most part, management strategies include a wait and see approach, reduction in medication dosage, switching medications, adjunct medications, cognitive behavioral therapy (CBT), and behavioral modifications (see the following subsections) (Table 3).25,28 Regardless of which management strategy a clinician employs, treatment should always follow an individualized, patient-centered approach, focusing primarily on minimizing SD without compromising the psychiatric well-being of the patient.28 Clinicians must also determine what strategies their patients have already tried to identify which treatments are more likely to be effective.28 Specifically regarding SSRI use, clinicians must educate their patients about the risks of PSSD.13,28 Although various management options for PSSD have been proposed, none have proven effective and there remains no definitive treatment.

Management Strategies
WAIT AND SEE. A wait and see approach may prove beneficial for some patients, as side effects from medications, particularly SSRIs, can dissipate over time. One study suggested that SD remits in 6 months for approximately 80% of patients, while others report remission in only 10%.25
MEDICATION REDUCTION. Another approach involves reduction in dosage, if feasible. SD related to antidepressants may be a dose-dependent adverse effect; therefore, reduction of dosage to a minimum effective dose may be beneficial. However, reduction in dosage could compromise the patient’s mental health, and depending on the particular medication, improvement in sexual function may take several months, which makes this strategy inappropriate for some patients.25 Moreover, many patients only require short-term courses of antidepressants, so in the appropriate setting, cessation of the medication altogether could be the best option.
DRUG HOLIDAYS. Although there is some evidence supporting the use of drug holidays (ie, temporarily discontinuing the drug on weekends), this may lead to withdrawal symptoms or medication nonadherence and is not recommended.25,29
CHANGING MEDICATIONS. Another strategy involves switching medications, in particular from an SSRI to a non-SSRI antidepressant. This may allow for the continuation of psychiatric treatment while potentially improving sexual function and adherence. For instance, switching to bupropion, an antidepressant with a favorable sexual side effect profile, has been used with success in patients with previous SSRI-induced SD,30 although these medications have their own unique set of side effects which, in some situations, may be even more distressing to the patient.28
INTERVENTIONS ADDRESSING SD. Augmentation strategies consisting of adding another pharmacological or psychotherapeutic treatment to counteract the psychotropic-related SD have shown success in some patients. Addition of bupropion, tamsulosin, phosphodiesterase-5 inhibitors (eg, sildenafil), testosterone, and 5-HT2 antagonists (eg, mirtazapine) to counteract SD without SSRI cessation can be an effective strategy for both men and women.1 CBT, sex therapy, couples counseling, acupuncture, and behavioral modifications such as the use of vibrators and scheduled sexual activity (ie, in the morning before the daily SSRI dose) have demonstrated mixed benefit.25,28
Concluding Thoughts
SD from psychiatric medications is relatively common. If a patient develops SD, multiple treatment strategies exist to help alleviate it. However, SD cannot be treated until it is first identified. Early, continuous, and direct conversations with patients about their sexual function is necessary—and should be anything but taboo.
Mr Drury is a medical student at Tulane University School of Medicine (TUSOM) pursuing urology. Mr Natale and Mr King are urology residents at TUSOM. Dr Hellstrom is a professor of urology and chief of the section of andrology at TUSOM. The authors note they have nothing to disclose regarding this article.
References
1. Lewis RW, Fugl-Meyer KS, Corona G, et al. Definitions/epidemiology/risk factors for sexual dysfunction. J Sex Med. 2010;7(4 Pt 2):1598-1607.
2. Harley EW, Boardman J, Craig T. Sexual problems in schizophrenia: prevalence and characteristics. A cross sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):759-766.
3. Montejo AL, Majadas S, Rico-Villademoros F, et al. Frequency of sexual dysfunction in patients with a psychotic disorder receiving antipsychotics. J Sex Med. 2010;7(10):3404-3413.
4. Bahrick AS. Post SSRI sexual dysfunction. Am Soc Adv Pharmacother Tablet. 2006;7:2-3.
5. Atmaca M. Selective serotonin reuptake inhibitor-induced sexual dysfunction: current management perspectives. Neuropsychiatr Dis Treat. 2020;16:1043-1050.
6. Stahl SM. Mechanism of action of serotonin selective reuptake inhibitors. Serotonin receptors and pathways mediate therapeutic effects and side effects. J Affect Disord. 1998;51(3):215-235.
7. Hirschfeld RM. Long-term side effects of SSRIs: sexual dysfunction and weight gain. J Clin Psychiatry. 2003;64(18):20-24.
8. Allen K, Baban A, Munjiza J, Pappa S. Management of antipsychotic-related sexual dysfunction: systematic review. J Sex Med. 2019;16(12):1978-1987.
9. Montejo AL, de Alarcón R, Prieto N, et al. Management strategies for antipsychotic-related sexual dysfunction: a clinical approach. J Clin Med. 2021;10(2):308.
10. Kaufman KR, Coluccio M, Linke M, et al. Alprazolam-induced dose-dependent anorgasmia: case analysis. BJPsych Open. 2018;4(4):274-277.
11. Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis. J Clin Psychopharmacol. 2009;29(3):259-266.
12. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
13. Bala A, Nguyen HMT, Hellstrom WJG. Post-SSRI sexual dysfunction: a literature review. Sex Med Rev. 2018;6(1):29-34.
14. Rappek NAM, Sidi H, Kumar J, et al. Serotonin selective reuptake inhibitors (SSRIs) and female sexual dysfunction (FSD): hypothesis on its association and options of treatment. Curr Drug Targets. 2018;19(12):1352-1358.
15. Safer DJ. Raising the minimum effective dose of serotonin reuptake inhibitor antidepressants: adverse drug events. J Clin Psychopharmacol. 2016;36(5):483-491.
16. Plevin D, Galletly C, Roughan P. Sexual dysfunction in men treated with depot antipsychotic drugs: a pilot study. Sex Health. 2007;4(4):269-271.
17. Serretti A, Chiesa A. A meta-analysis of sexual dysfunction in psychiatric patients taking antipsychotics. Int Clin Psychopharmacol. 2011;26(3):130-140.
18. Park EJ, Amatya S, Kim MS, et al. Long-acting injectable formulations of antipsychotic drugs for the treatment of schizophrenia. Arch Pharm Res. 2013;36(6):651-659.
19. Novick D, Haro JM, Perrin E, Suarez D, et al. Tolerability of outpatient antipsychotic treatment: 36-month results from the European Schizophrenia Outpatient Health Outcomes (SOHO) study. Eur Neuropsychopharmacol. 2009;19(8):542-550.
20. Bobes J, Garc A-Portilla MP, Rejas J, et al. Frequency of sexual dysfunction and other reproductive side-effects in patients with schizophrenia treated with risperidone, olanzapine, quetiapine, or haloperidol: the results of the EIRE study. J Sex Marital Ther. 2003;29(2):125-147.
21. Márquez M, Arenoso H, Caruso N. Efficacy of alprazolam sublingual tablets in the treatment of the acute phase of panic disorders. Actas Esp Psiquiatr. 2011;39(2):88-94.
22. Fava M, Borofsky GF. Sexual disinhibition during treatment with a benzodiazepine: a case report. Int J Psychiatry Med. 1991;21(1):99-104.
23. Rosenberg KP, Bleiberg KL, Koscis J, Gross C. A survey of sexual side effects among severely mentally ill patients taking psychotropic medications: impact on compliance. J Sex Marital Ther. 2003;29(4):289-296.
24. Rizvi SJ, Yeung NW, Kennedy SH. Instruments to measure sexual dysfunction in community and psychiatric populations. J Psychosom Res. 2011;70(1):99-109.
25. Lorenz T, Rullo J, Faubion S. Antidepressant-induced female sexual dysfunction. Mayo Clin Proc. 2016;91(9):1280-1286.
26. Shindel A, Althof S, Carrier S, et al. Disorders of ejaculation: an AUA/SMSNA guideline. American Urological Association Website. Accessed Jan 28, 2021. https://www.auanet.org/guidelines/disorders-of-ejaculation
27. Hatzimouratidis K, Giuliano F, Moncada I, et al. Male sexual dysfunction. European Association of Urology Website. Accessed Jan 28, 2021. https://uroweb.org/guideline/male-sexual-dysfunction/
28. Higgins A, Nash M, Lynch AM. Antidepressant-associated sexual dysfunction: impact, effects, and treatment. Drug Healthc Patient Saf. 2010;2:141-150.
29. Rothschild AJ. Selective serotonin reuptake inhibitor-induced sexual dysfunction: efficacy of a drug holiday. Am J Psychiatry. 1995;152(10):1514-1516.
30. Zajecka J. Strategies for the treatment of antidepressant-related sexual dysfunction. J Clin Psychiatry. 2001;62 Suppl 3:35-43.❒
FUENTE: www.psychiatrictimes.com